The programme
08:30
Registration and Breakfast
Registration - Open from 8:30am - Closes at 10:30 am
All delegates must complete their registration process before the 10:30 AM cut-off time. Please arrive in a timely manner to allow for registration and to avoid any inconvenience. Delegates who arrive after the registration deadline will be refused entry to the event.
We appreciate your cooperation in helping us maintain the event's schedule and ensuring that everyone can fully participate in the Virtual Wards Conference. If you have any questions or require assistance, our event staff will be available to assist you with the registration process.
Thank you for your understanding, and we look forward to an insightful and productive event together!
09:30
Chair Opening Address (Confirmed)
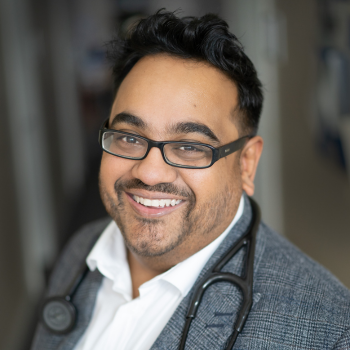
Dr Gurnak Singh Dosanjh
GP
LLR ICB
Chair Opening Address (Confirmed)
09:40
Keynote Presentation - The Medway and Swale Virtual Hospital – taking technology led virtual wards to the next level (Confirmed)
Tracy Stocker
Director of Operations for Flow and Integration
Medway NHS Foundation Trust
This initiative focuses on actively engaging patients, carers, and clinicians to co-create and implement optimal virtual healthcare services. By integrating these perspectives, the Virtual Hospital aims to enhance patient flow, boost clinical effectiveness, and deliver a seamless, patient-centered care experience across the entire healthcare system.
10:00
Optimising Integrated Care: Developing Comprehensive Virtual Ward Plans Panel Discussion
Francesca Markland
Senior Programme Manager, Remote Monitoring & Virtual Wards
NHSE London Region Digital Transformation Team
Adam Fitzgerald
Head of Nursing, Integrated Local Services
Guy’s and St Thomas’ NHS Foundation Trust
Dr Reggie Sangha
Content Guru
Medical Director
Greg Edwards
Chief Medical Officer
Doccla
Clare Evans
Care Co-ordination and Hospital@Home Programme Manager
Bath, Swindon & Wiltshire ICB
This panel discussion delves into the imperative for Integrated Care Systems (ICS) to formulate thorough plans for virtual wards, emphasising key components such as Pathways, Governance, and patient safety. Experts will explore the definition and objectives of virtual wards within ICS, discussing the integration of healthcare services, robust governance frameworks, and strategies for ensuring patient safety. The conversation will also cover technology requirements, workforce training, patient-centred care approaches, and methods for measuring success. By addressing these critical elements, the panel aims to equip ICS with the insights and strategies needed to effectively implement virtual wards, enhancing patient outcomes and driving innovation in healthcare delivery.
Panellists:
-
Francesca Markland, Senior Programme Manager, Remote Monitoring & Virtual Wards, NHSE London Region Digital Transformation Team (Confirmed)
-
Greg Edwards, Chief Medical Officer, Doccla (Confirmed)
-
Dr Reggie Sangha, Medical Director, Content Guru (Confirmed)
- Adam Fitzgerald, Head of Nursing – Integrated Local Services, Guy’s and St. Thomas’ NHS Foundation Trust (Confirmed)
- Clare Evans, Care Co-ordination and Hospital@Home Programme Manager, Bath, Swindon & Wiltshire ICB (Confirmed)
10:30
Main Sponsor - Scaling Virtual Wards: Revolutionizing Patient Care
Dr Reggie Sangha
Content Guru
Medical Director
Main Sponsor - Content Guru
The NHS is under immense pressure, facing budget constraints and capacity challenges in a tough economic climate. In line with the new Labour government’s mission to build a NHS ‘fit for the future’, integrating technology has become more critical than ever. A promising solution? Large-scale Virtual Wards.
Although initial central funding for Virtual Wards has ended, they have proven to deliver significant cost savings and efficiencies. As the NHS targets 50 beds per 100,000 people, effectively scaling Virtual Wards to ensure they become a self-funding proposition is crucial.
Join Reggie Sangha, Medical Director at Content Guru & a Doctor within the NHS, for a comprehensive guide on scaling Virtual Wards, where she will showcase successful examples of patient engagement, data orchestration, and interoperability to ensure these initiatives thrive financially and support the NHS’s goals.
11:50
Chair Morning Reflection (Confirmed)
Dr Gurnak Singh Dosanjh
GP
LLR ICB
Chair Morning Reflection (Confirmed)
11:55
Case Study - Unlocking the Future of Virtual Wards: Integration and Innovation in Community Care
Laura Thompson
Director of Marketing
Access Group
Deborah Snook
Integrated Care Consultant
Access Group
Case Study - Access
This talk will provide an update on the NELFT programme's progress in creating truly integrated virtual wards, highlighting successes in collaboration, technology, and patient outcomes. It will explore future strategies for enhancing step-up capabilities, building on the success of step-down virtual wards, emphasizing the importance of seamless integration across health systems to ensure effective community-first responses.
12:15
Case Study - Proactive Heart Failure Management: A Case Study of the MHF@Home Programme
Dr Maha Balakrishnan
GP and Hospital at Home Clinical Lead
Case Study - Doccla
Join us for an insightful case study presentation on the Managing Heart Failure @Home (MHF@Home) programme, a collaboration between East and North Hertfordshire NHS Trust, Hertfordshire Community Trust, and Doccla. Over six months, the pilot supported 52 heart failure patients with remote monitoring and personalised self-management, resulting in a complete reduction in 30-day readmissions and saving £6,822. Patients saw improvements in mobility, self-care, and overall quality of life, with health scores rising from 63 to 71 on the VAS scale. Discover how this proactive care model can transform chronic disease management and reduce healthcare pressures.
12:35
Fireside Interview - Challenges in scaling and maturity within virtual wards (Confirmed)
Francesca Markland
Senior Programme Manager, Remote Monitoring & Virtual Wards
NHSE London Region Digital Transformation Team
12:55
Case Study - Ortus iHealth
Dr. Debashish Das
Consultant Cardiologist Barts NHS Trust
CEO & Founder Ortus-iHealth
Case Study - Ortus iHealth
Dr Debashish Das invites us to rethink the current approach to virtual wards by exploring the transformative potential of long-term remote monitoring for chronic conditions. Challenging the limitations of confining patient care to a two-week virtual ward stay, he emphasises that long-term conditions require continuous support beyond short-term interventions.
Drawing on examples from Bart’s NHS Trust and Ortus-iHealth—including heart failure virtual wards and remote medicines optimisation—Dr Das will illustrate how proactive remote monitoring can be seamlessly integrated into existing clinical pathways. He will delve into the evidence supporting remote monitoring in heart failure, underscoring the necessity of delivering virtual care through evidence-based interventions.
By considering the entire patient journey, Dr Das will demonstrate how continuous remote care can prevent hospital admissions, reduce the need for acute interventions, and enhance patient outcomes. Aligning with the anticipated NHS focus on moving "from analogue to digital and from hospital to community," we will explore how we have taken that forward in our heart failure patients
14:00
Chair Afternoon Address (Confirmed)
Dr Gurnak Singh Dosanjh
GP
LLR ICB
Chair Afternoon Address (Confirmed)
14:05
Case Study - NHS and Care Volunteer Responders: Adding capacity to Virtual Ward Teams
Ben Long
Programme Manager, NHS and Care Volunteer Responders
Royal Voluntary Service
Case Study - Royal Voluntary Service
NHS and Care Volunteer Responders: Adding capacity to Virtual Ward Teams
The NHS and Care Volunteer Responders programme is a unique partnership between NHS England, Royal Voluntary Service, and tech platform GoodSAM with over 43,000 ID-Checked volunteers available to support healthcare teams across England.
Volunteers can support Virtual Ward Teams through the Pick Up and Deliver Service. This free service ensures prompt delivery of medications, equipment, and mobility aids to patients being cared for on a virtual ward, allowing teams to focus on critical tasks and patient care. Additionally, it contributes to NHSE's Net Zero goals by facilitating the collection and redistribution of mobility aids, reducing waste and environmental impact.
Join us to discover how this invaluable volunteer service can enhance your Virtual Ward team's efficiency and improve patient care.
14:25
The Role of NHS Workforce Long-Term Plan in Advancing Virtual Ward Services and Building a Resilient Healthcare Workforce Panel Discussion
Dr Raees Lunat
Chief Medical Information Officer, GP Registrar and ex Senior Advisor to the Chief Workforce Officer of the NHS
West Hertfordshire Trust
Jen Tomkinson
Associate Director NHS@home
Sirona care & health
Adam Fitzgerald
Head of Nursing, Integrated Local Services
Guy’s and St Thomas’ NHS Foundation Trust
Dr. Matea Deliu
Academic GP, Clinical Lead Digital Delivery, Clinical Safety Officer
NHS South East London ICB
In this panel discussion, we're exploring the vital link between the NHS Workforce Long-Term Plan and the evolution of virtual care, particularly focusing on the expansion of virtual ward services. We will emphasise how these initiatives align with the changing landscape of healthcare delivery, stressing the importance of workforce recruitment and digital proficiency among healthcare professionals. By prioritising workforce development, healthcare organisations can ensure the delivery of high-quality virtual care services, ultimately reshaping healthcare delivery into a more resilient and patient-centric model.
Panellists:
-
Dr Raees Lunat, Chief Medical Information Officer, GP Registrar and ex Senior Advisor to the Chief Workforce Officer of the NHS West Hertfordshire Trust (Confirmed)
- Adam Fitzgerald, Head of Nursing – Integrated Local Services, Guy’s and St. Thomas’ NHS Foundation Trust (Confirmed)
-
Dr. Matea Deliu, Associate Medical Director, One Health Lewisham (Confirmed)
14:45
Case Study - Transforming Remote Healthcare Delivery - COPD Virtual Wards and the Healthy Islands Project
Dr Ian McCabe
Research Fellow and Project Manager, Hive Lab, University of Galway
University of Galway
Ciara Gormley
Customer Success Manager
myPatientSpace
myPatientSpace Case Study: Transforming Remote Healthcare Delivery - COPD Virtual Wards and the Healthy Islands Project
Overview:
Galway University Hospital (GUH), in partnership with MyPatientSpace, HSE, and Cisco, is advancing remote healthcare through two groundbreaking projects: the COPD Virtual Ward and the Healthy Islands initiative. Both programs leverage telehealth and digital health platforms to overcome barriers to care, significantly impacting patient outcomes in remote and underserved areas.
1. COPD Virtual Ward: Revolutionizing Chronic Disease Management
The COPD Virtual Ward at GUH addresses the needs of patients with chronic obstructive pulmonary disease (COPD). Using MyPatientSpace, patients can monitor symptoms, oxygen levels, and vital signs from home, reducing hospital visits and allowing clinicians to intervene early when issues arise. In the first 10 weeks of its launch, the program saved over 205 bed days and aligns with Ireland’s Sláintecare strategy to enhance patient-centered care.
2. Healthy Islands Project: Bridging Gaps in Remote Island Healthcare
The Healthy Islands Project extends this model to the isolated communities on Clare Island, Inishturk, and Inishbofin, where limited access to GPs has posed a longstanding challenge. Telehealth tools and MyPatientSpace allow nurses on these islands to collect vital patient data, which mainland doctors can review in real time, thus providing timely and consistent care. The project also supported remote hypertension management and consultant led virtual care. The project also adapts the COPD virtual care pathway to serve island residents, ensuring they receive specialized care without leaving their communities.
Key Outcomes and Impact
Both initiatives transform healthcare delivery by:
Enhancing Access: Bringing continuous and proactive care to patients’ homes, even in geographically isolated regions.
Improving Outcomes: Early detection and real-time monitoring reduce emergency admissions and hospital stays.
Increasing Patient Satisfaction: Patients report a greater sense of security and empowerment in managing their health and staying at home.
Conclusion:
Galway University Hospital’s collaboration with MyPatientSpace demonstrates the potential of virtual healthcare pathways to deliver patient-centric, accessible care in both urban and rural settings and next generation Virtual Hospital models. These initiatives are models for scalable, remote healthcare solutions that can serve as a blueprint for other regions facing similar challenges, and closely reflecting the NHS Virtual Ward framework by enhancing patient-centered, technology-enabled care in the community
15:05
Pioneering a digitally first virtual ward in South East London (Confirmed)
Dr. Matea Deliu
Academic GP, Clinical Lead Digital Delivery, Clinical Safety Officer
NHS South East London ICB
Pioneering a digitally first virtual ward in South East London
15:25
Keynote Presentation - Working towards an Integrated Regional Virtual Hospital (Confirmed)
Mr Mike Waters
Operational Lead Virtual Ward
Norfolk & Norwich University Hospital
How we hope to achieve our goal of a regional Virtual Hospital.
15:45
Hot Buffet Food & Drinks Reception
Hot Buffet Food & Drinks Reception